Liudmila Benni
Moldova
DMARD treatment of rheumatoid arthritis
Liudmila Benni, Elena Deseatnicova
Abstract
Background
Rheumatoid arthritis (RA) is a chronic autoimmune disease characterized by joint inflammation, progressive structural damage, and systemic complications. Disease-modifying anti-rheumatic drugs (DMARDs) form the cornerstone of RA treatment, aiming to control disease activity and prevent long-term joint damage. Conventional synthetic DMARDs (csDMARDs), such as methotrexate, remain the first-line therapy. However, biological DMARDs (bDMARDs) and targeted synthetic DMARDs (tsDMARDs) expand therapeutic options. Recent research has focused on optimizing bDMARD dosing in patients in remission, comparing the efficacy of bDMARDs and tofacitinib, and integrating patient-centered decision-making tools.
Methods
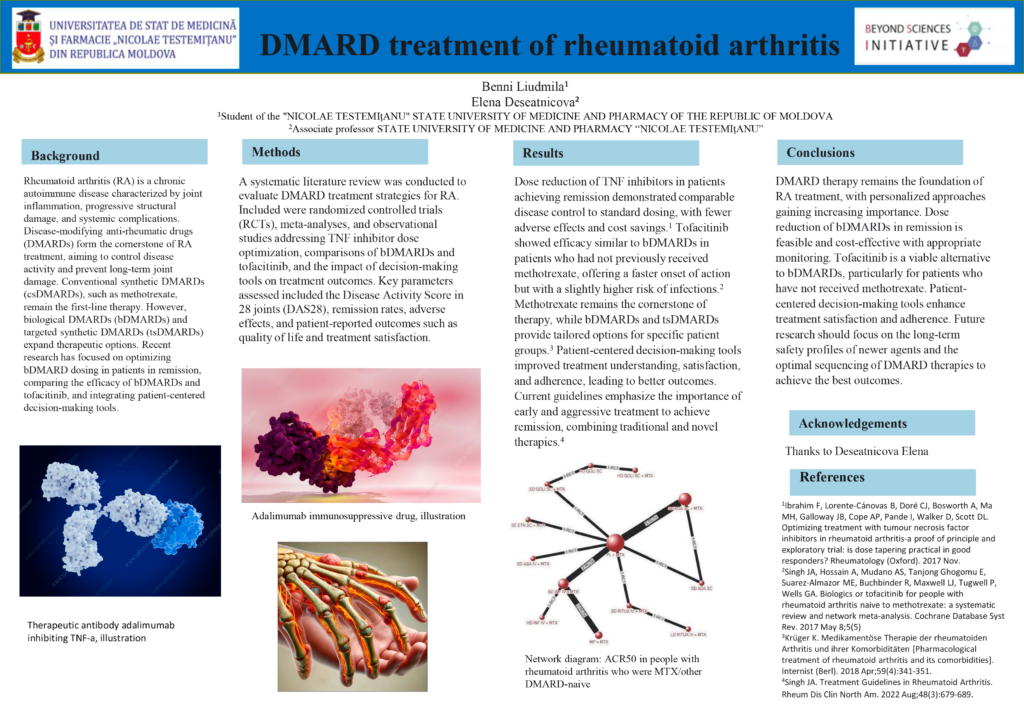
A systematic literature review was conducted to evaluate DMARD treatment strategies for RA. Included were randomized controlled trials (RCTs), meta-analyses, and observational studies addressing TNF inhibitor dose optimization, comparisons of bDMARDs and tofacitinib, and the impact of decision-making tools on treatment outcomes. Key parameters assessed included the Disease Activity Score in 28 joints (DAS28), remission rates, adverse effects, and patient-reported outcomes such as quality of life and treatment satisfaction.
Results
Dose reduction of TNF inhibitors in patients achieving remission demonstrated comparable disease control to standard dosing, with fewer adverse effects and cost savings. Tofacitinib showed efficacy similar to bDMARDs in patients who had not previously received methotrexate, offering a faster onset of action but with a slightly higher risk of infections. Methotrexate remains the cornerstone of therapy, while bDMARDs and tsDMARDs provide tailored options for specific patient groups. Patient-centered decision-making tools improved treatment understanding, satisfaction, and adherence, leading to better outcomes. Current guidelines emphasize the importance of early and aggressive treatment to achieve remission, combining traditional and novel therapies.
Conclusions
DMARD therapy remains the foundation of RA treatment, with personalized approaches gaining increasing importance. Dose reduction of bDMARDs in remission is feasible and cost-effective with appropriate monitoring. Tofacitinib is a viable alternative to bDMARDs, particularly for patients who have not received methotrexate. Patient-centered decision-making tools enhance treatment satisfaction and adherence. Future research should focus on the long-term safety profiles of newer agents and the optimal sequencing of DMARD therapies to achieve the best outcomes.

Leave A Comment