Rania Mohamed
Egypt
The diabetic type 2 microenvironment deteriorates the gamma delta T cell function
Rania Hassan Mohamed1, Ali E. Elhargy2, Shireen Magdy2, Abd ElRahman Abouzid2, Nagwa ElBadry2
1. Department of Biochemistry, Faculty of Science, Ain Shams University, Cairo, Egypt
2. Center of Excellence for Stem Cells and Regenerative Medicine, Zewail City of Science and technology, Giza, Egypt
Abstract
Background
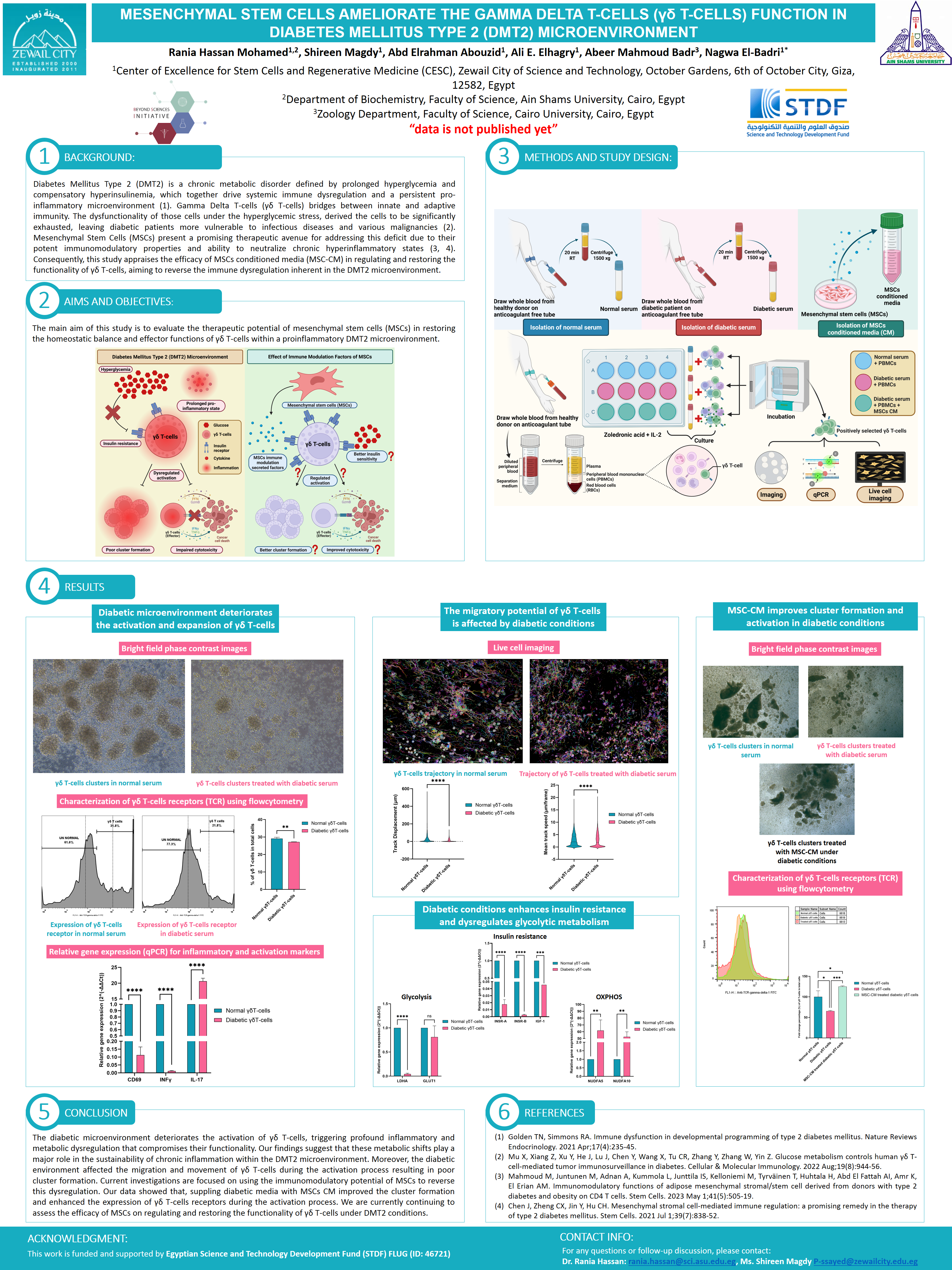
Diabetes mellitus type 2 (DMT2) is a chronic metabolic disorder that characterized by prolonged hyperglycemia and compensatory hyperinsulinemia. Beyond metabolic dysfunction, DMT2 is associated with immune dysregulation affecting both innate and adaptive immunity levels, contributing to the establishment of chronic inflammatory microenvironment. Gamma-delta T-lymphocytes (γδ T-cells) have been reported to be dysregulated under hyperglycemic conditions. However, the exact mechanism by which hyperglycemic microenvironment alter the functionality of δγ T-cells are still poorly understood. Mesenchymal stem cells (MSCs) were reported to be promising therapeutic agent for modulating the chronic inflammation of DMT2 microenvironment owing to their anti-inflammatory potential that neutralize the chronic hyperinflammatory state. Based on this fact, we appraise the efficacy of MSCs conditioned media on regulating and restoring the functionality of γδ T-cells under DMT2 conditions.
Methods
Gamma 9 delta 2 T (γ9δ2 T) cells were isolated from the blood of healthy individuals, then expanded and activated in the presence of the diabetic or normal microenvironment. The activation and metabolic status were assessed using imaging, flow cytometry, QPCR and functionality assays on positively selected gamma delta T cells using flow sorting.
Results
The γδ T cells failed to form appropriate activated clusters after treatment with the diabetic microenvironment, which decreased the activation as shown by the downregulated expression of CD69 activation marker, and decreased the number of γδ T cells. The diabetic microenvironment also increased the pro-inflammatory subsets more than the normal microenvironment as observed by higher IL-17 over IFNγ expression. Also, the metabolic status of the γδ T cell is also disrupted to be less glycolytic, which is relevant to the pro-inflammatory subset.
Conclusions
The diabetic microenvironment disrupted both inflammatory and metabolic conditions of the γδ T cells, which deteriorates their functionality. We are currently assessing the efficacy of MSCs on regulating and restoring the functionality of γδ T-cells under DMT2 conditions.

Leave A Comment