Mustak Ahamed
India
Evaluation of Antibiotic Prescribing Patterns in Surgical Prophylaxis at a Public Sector Hospital
Mustak Ahamed¹*, Garry Hunjan¹, Dr. Khadga Raj Aran¹
1Department of Pharmacy Practice, ISF College of Pharmacy (An Autonomous College), Moga-142001, Punjab, India.
Abstract
Background
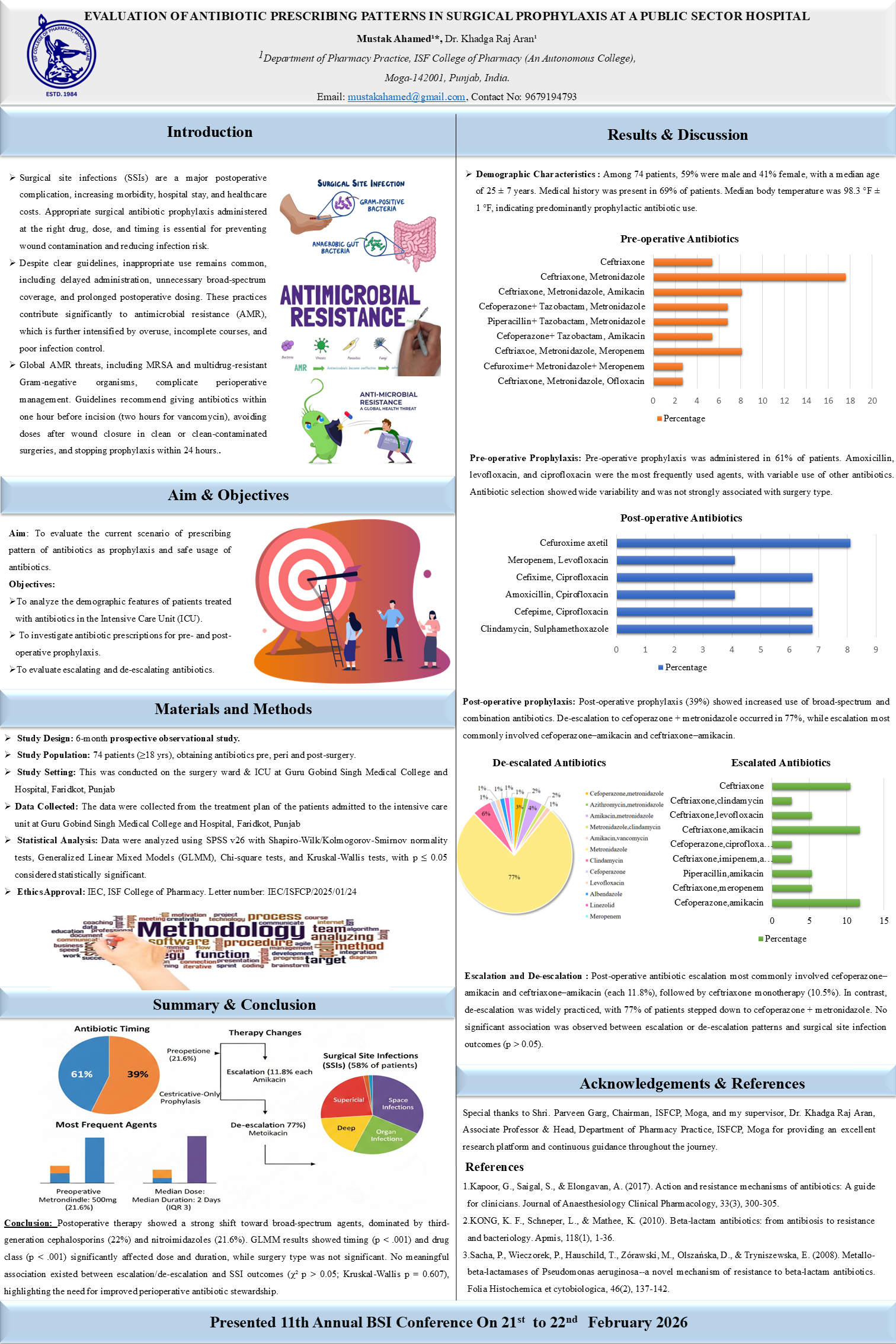
Surgical site infections (SSIs) play a major role in postoperative morbidity, hospitalization, and excessive healthcare expenses. Rational antibiotic prophylaxis is essential to reduce the risk of infections and to avoid antimicrobial resistance. The objective of the study was to analyze the patterns of prescribing antibiotics as surgical prophylaxis and determine the rates of escalation and de-escalation in a state-funded hospital in Punjab.
Methods
The prospective observational study was carried out within a period of six months in the surgical wards of Guru Gobind Singh Medical College and Hospital, Faridkot. A total of 77 patients who received antibiotics either pre-, peri, or post-surgery were included based on the inclusion and exclusion criteria. SPSS version 30 was used to analyze data on the type of antibiotic used, time, duration, and clinical outcome. The Chi-square and Kruskal-Wallis tests were used to determine relations between antibiotic modification and the occurrence of surgical site infections.
Results
Out of 77 patients, 56% were male and 44% female, with an average age of 45.6 + 12.4 years. Ceftriaxone (41%) was prescribed most frequently as a prophylactic (ted) with amoxicillin-clavulanate (26%), and then with piperacillin-tazobactam (15%). The escalation of antibiotic therapy was detailed in 32.4 percent of cases, mostly because of the intraoperative contamination or the extended length of the surgical operation, and de-escalation was noted in 40.2 percent of the patients after the culture and sensitivity outcomes. The total incidence of SSI was 13% and the relationship between a long period of postoperative antibiotic therapy and SSI was statistically significant (p < 0.05). The average length of stay in patients who received de-escalation (6.1 + -1.4 days) was less than that of patients who experienced escalation (9.0 + -2.0 days).
Conclusions
The research shows significant non-conformity to the recommended surgical antibiotic prophylaxis protocols, especially in terms of duration and continuance after surgery. Culture-based de-escalation minimized the occurrence of SSI as well as hospitalization and antibiotics. Enhancing the adoption of antibiotic stewardship practices in the surgical environment can improve treatment outcomes and prevent antimicrobial resistance.

Leave A Comment