Goeun Lee
Conference 2022 Poster Presentation
Project title
HPV type distribution in women in Toronto and comparison of HPV testing versus Pap smear as the primary screening test for cervical cancer.
Authors and Affiliations
Goeun Lee1, Seung Hee Han2,3
1. Department of Microbiology and Immunology, University of Toronto, Toronto, Canada
2. Department of Medical Biophysics, Faculty of Medicine, University of Toronto, Toronto, Canada
3. Princess Margaret Cancer Center, University Health Network, Toronto, Canada
Abstract
Background
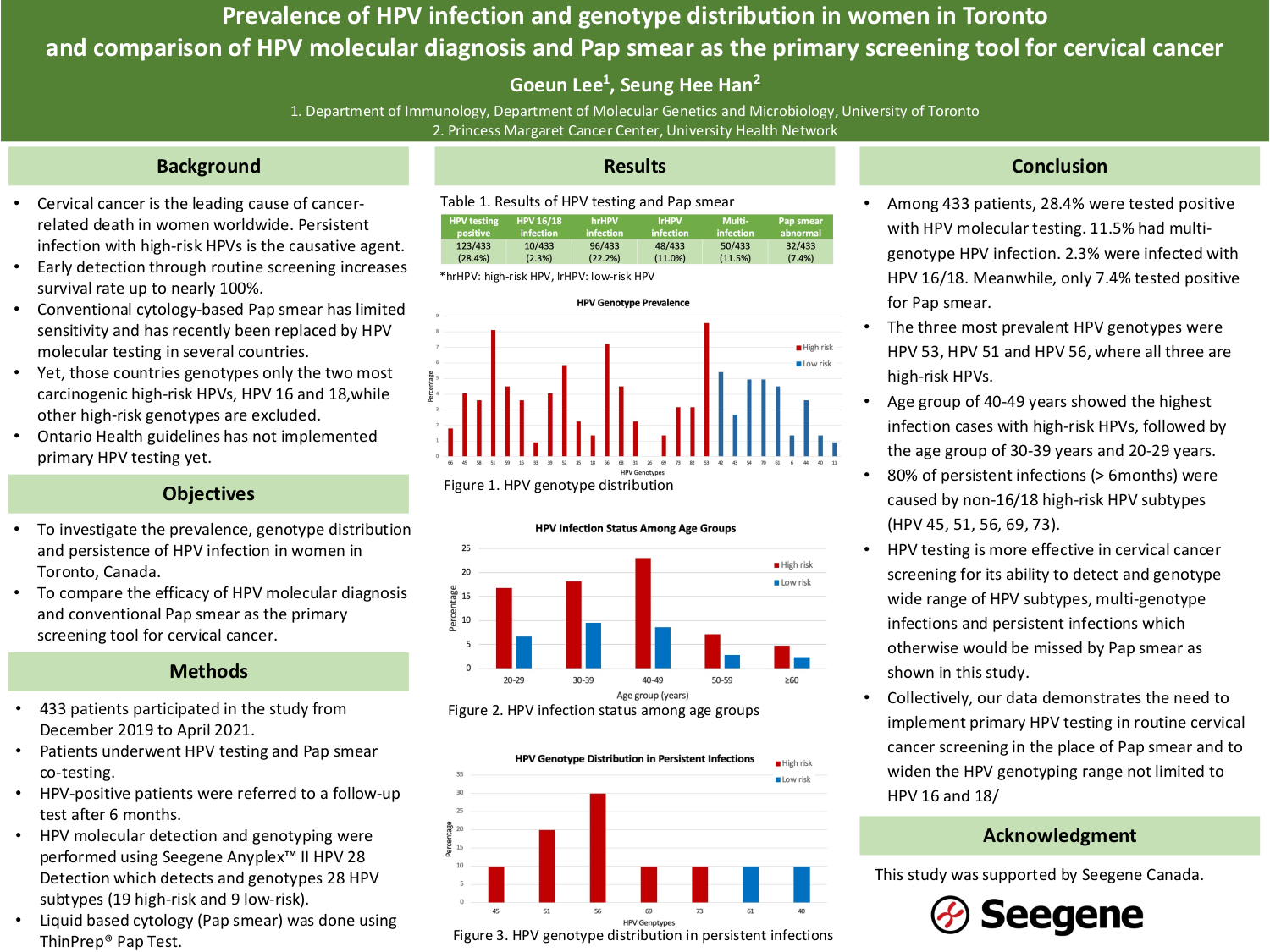
Cervical cancer is the leading cause of cancer-related death in women worldwide, and infection with high-risk HPV is the causative agent. Since the survival rate goes up to nearly 100% with early detection, routine screening plays an essential role in reducing the burden of cervical cancer. For its higher sensitivity compared to conventional cytology-based Pap smear, some countries have implemented primary HPV testing as the screening tool for cervical cancer, although only the two most carcinogenic high-risk HPV types, HPV 16 and 18, are genotyped while other high-risk subtypes are excluded. Also, Ontario Ministry of Health guidelines has not implemented primary HPV testing yet. In this study, we investigated the HPV prevalence and type distribution in women in Toronto, Canada and compared the compatibility of HPV testing versus Pap smear as the primary screening tool for cervical cancer.
Methods
361 women were recruited from Toronto, Canada from August 2019 and November 2021, and underwent HPV testing and Pap smear co-testing. HPV testing was done using Seegene Anyplex™ II HPV 28 Detection which detects and genotypes 28 HPV subtypes. HPV-positive individuals were referred to follow-up HPV tests in 3-month and 6-month interval. Then, the sensitivity and specificity of HPV testing and Pap smear was compared. Moreover, the prevalence of HPV and the genotype distribution were assessed.
Results
Our study showed that 27% of the participants were HPV-positive. HPV testing had higher sensitivity and lower specificity compared to Pap smear. Moreover, infection with HPV 16 and 18 account for only 6.8% of all positive cases, while 58.6% was with low risk HPVs, and the remaining 34.6% was with non-16/18 high risk HPVs. Also, some of the non-HPV 16/18 infection persisted for subsequent follow-up tests.
Conclusions
These findings suggest that HPV testing detects HPV infection with higher sensitivity compared to conventional Pap smear. More importantly, the data demonstrates a need to implement primary HPV testing and broadening the HPV genotyping range in routine screening, although subsequent follow-ups are needed to investigate if the persistent infection of non-16/18 HPVs eventually leads to cervical cancer.