Maureen Kemuma Bikoro
Conference 2023 Presentation
Project title
Non-cardiac cormobidities among heart failure patients admitted at Moi Teaching and Referral Hospital, Eldoret, Kenya
Authors and Affiliations
Bikoro Maureen1, Barasa Felix2, Oduor Chrispine3
1. Department of Medicine, Moi University, Eldoret, Kenya
2. Department of Cardiology, Moi Teaching and Referral Hospital, Eldoret, Kenya
3. Department of Medicine, Moi University, Eldoret, Kenya
Abstract
Background
Heart failure (HF) in Sub-Saharan Africa (SSA) is on the upsurge as a result of epidemiologic and demographic transition to those of high-income countries.
HF mostly affects the young and middle aged who present in New York Heart Association (NYHA) class IV and have no health insurance. Non-Cardiac Comorbidities (NCC), defined as additional non-cardiac diseases co-existing with Heart Failure (HF), have been independently associated with acceleration of disease progression, poor response to treatment, mortality, hospitalization, re-hospitalization rates, poor health related quality of lifeandearlydisability. Despite use of novel therapies in HF,which focus on improvement of cardiovascular status, there has been minimal improvement in outcomes which may partly be attributed to combined effect of NCC.
Methods
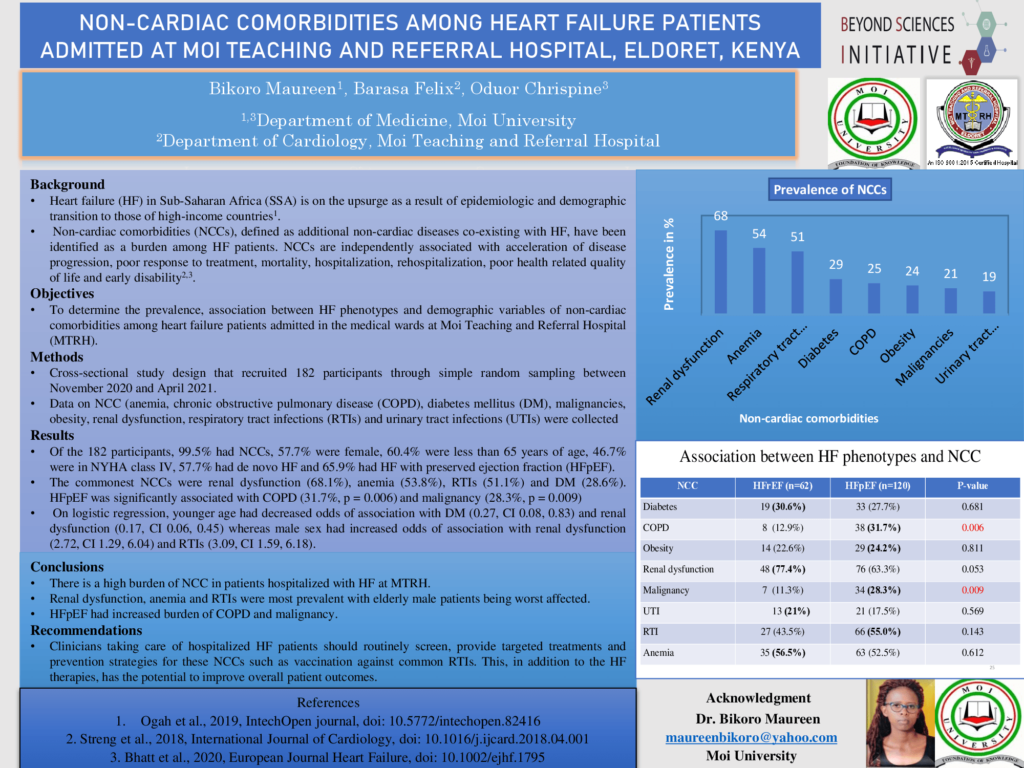
Cross-sectional study design that recruited 182 participants through simple random sampling. An interviewer administered structured questionnaire was used to obtain participants demographic characteristics and NCCs (anemia, COPD, DM, malignancies, obesity, renal dysfunction, respiratory tract infections (RTIs) and urinary tract infections (UTIs) and participants demographic characteristics were collected. Chi- square, fishers exact and logistic regression analyses were performed to test for association between NCC, HF phenotypes and demographic characteristics.
Results
Out of the 182 participants, 57.7% were female, 60.4% were less than 65 years of age, 46.7% were in NYHA class IV, 57.7% had de novo HF and 65.9% had HFpEF. HFpEF was significantly associated with COPD (31.7%,p=0.006) and malignancy (28.3%, p = 0.009). On logistic regression, younger age had decreased odds of association with DM (0.27, CI 0.08, 0.83) and renal dysfunction (0.17, CI 0.06, 0.45) whereas male sex had increased odds of association with renal dysfunction (2.72, CI 1.29, 6.04) and RTIs (3.09, CI 1.59, 6.18).
Conclusions
There is a high burden of NCC in patients hospitalized with HF at Moi Teaching and Referral Hospital (MTRH). Renal dysfunction, anemia and RTIs were most prevalent with elderly male patients being worst affected. HFpEF had increased burden of COPD and malignancy. HFpEF had increased burden of COPD and malignancy. We recommend that routine screening, provision of targeted treatments and vaccination against common RTIs in addition to HF therapies has the potential to improve overall outcomes.