Saba Farooq Farooq
Pakistan
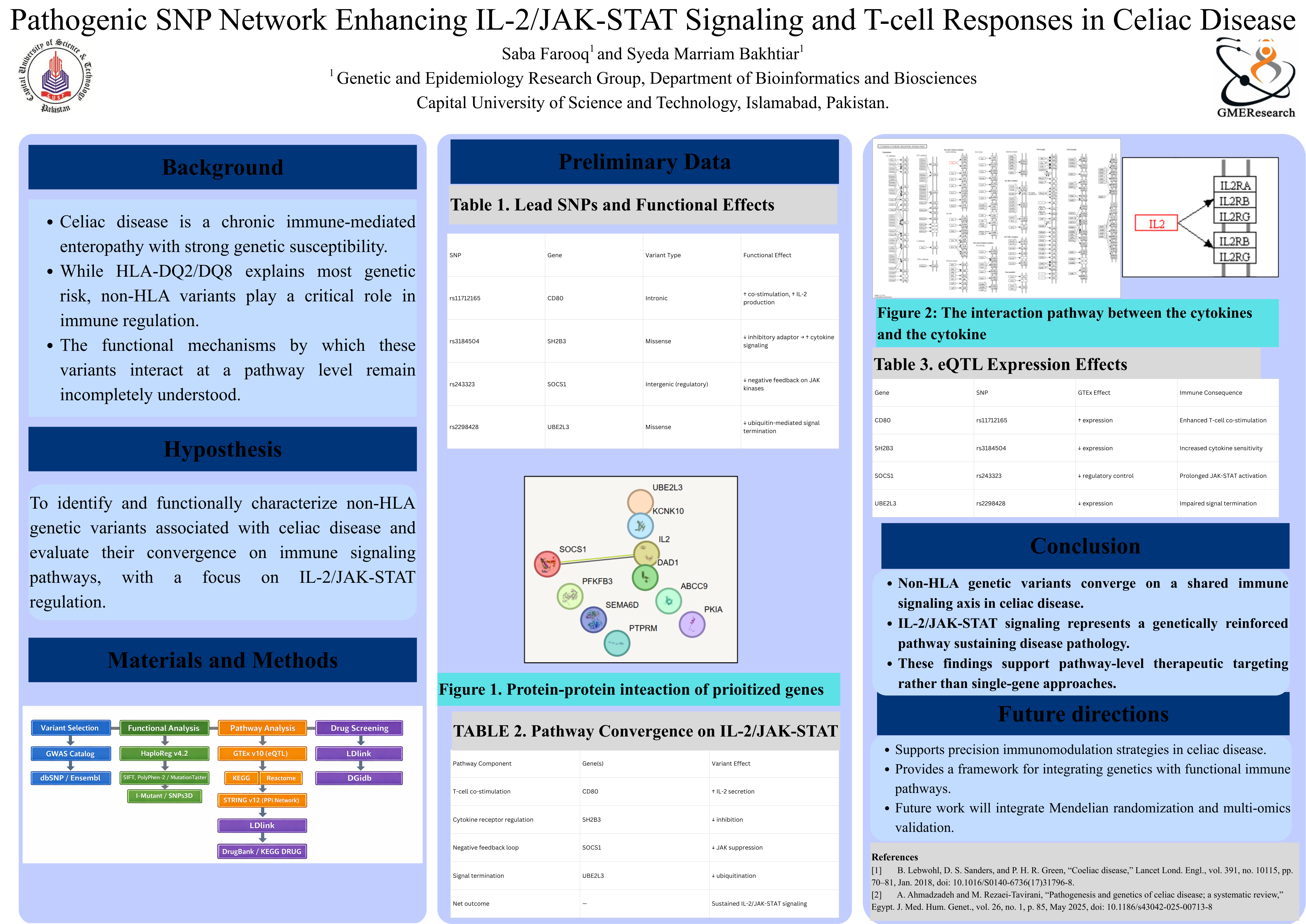
Pathogenic SNP Network Enhancing IL-2/JAK-STAT Signaling and T-cell Responses in Celiac Disease
Saba Farooq1 and Syeda Marriam Bakhtiar1*
1. Genetic and Epidemiology Research Group, Department of Bioinformatics and Biosciences, Capital University of Science and Technology, Islamabad, Pakistan.
Abstract
Background
Celiac disease is an immune-mediated enteropathy characterized by aberrant T-cell activation in response to dietary gluten. While HLA-DQ2/DQ8 molecules account for major genetic susceptibility, they do not fully explain the heightened cytokine responsiveness and chronic inflammation observed in many patients. Emerging evidence indicates that non-HLA immune-regulatory genes may amplify key signaling pathways, particularly the IL-2/JAK-STAT axis, which is known to be disproportionately activated during gluten exposure.
Methods
An integrative bioinformatics workflow was used to evaluate four immune-regulatory SNPs: rs11712165 (CD80), rs3184504 (SH2B3), rs243323 (SOCS1), and rs2299482 (UBE2L3). Analyses included functional annotation, GTEx eQTL expression profiling, KEGG pathway mapping, linkage disequilibrium assessment, and drug–gene interaction screening. Expression direction and regulatory impact were combined to construct a mechanistic model connecting these variants to cytokine signaling dysregulation.
Results
CD80 upregulation was associated with enhanced co-stimulation and increased IL-2 secretion, while reduced SH2B3 expression diminished inhibitory adaptor activity, promoting cytokine hyperresponsiveness. Lower SOCS1 expression weakened negative feedback on JAK kinases, and reduced UBE2L3 expression impaired ubiquitin-mediated signal termination. Together, these alterations converged to amplify IL-2/JAK-STAT signaling, resulting in sustained T-cell activation consistent with celiac disease immunopathology. Drug interaction screening identified CD80-targeting agents and multiple JAK inhibitors as potential pathway-specific modulators.
Conclusions
This study demonstrates that non-HLA SNPs in CD80, SH2B3, SOCS1, and UBE2L3 synergistically enhance IL-2/JAK-STAT signaling and contribute to the chronic inflammatory environment characteristic of celiac disease. The findings highlight the importance of non-HLA genetic architecture in disease progression and provide a mechanistic framework for identifying targeted therapeutic strategies.

Leave A Comment