Fatima Zahrae Bartal
Morocco
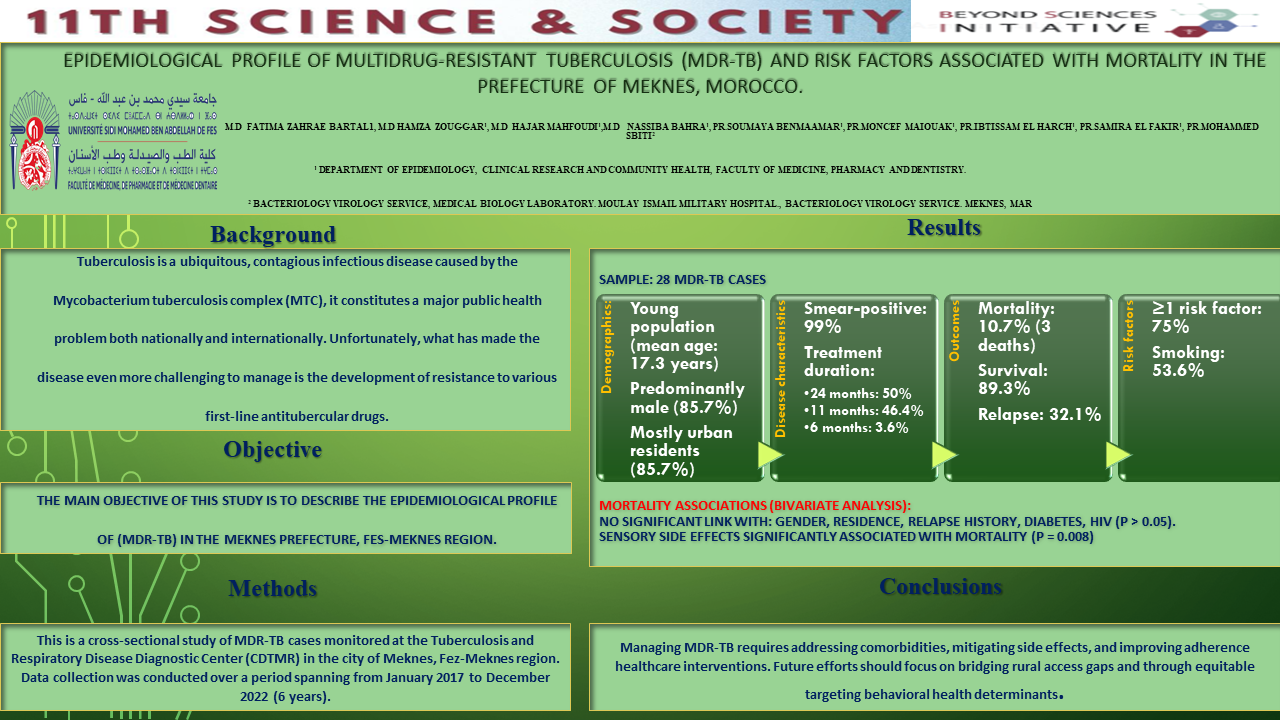
Epidemiological Profile of Multidrug-Resistant Tuberculosis (MDR-TB) and Risk Factors Associated with Mortality in the Prefecture of Meknes, Morocco
Fatima Zahrae Bartal12, Hamza Zouggar1, Hajar Mahfoudi12, Nassiba Bahra12, Soumaya Benmaamar12, Moncef Maiouak12, Ibtissam El Harch12, Samira El Fakir12, Mohammed Sbiti3
1 Department of Epidemiology, Clinical Research and Community Health, Faculty of
Medicine, Pharmacy and Dentistry.
2 Laboratory of Epidemiology and Research in Health Sciences, Sidi Mohamed Ben Abdellah University, Fez, Morocco.
3 Bacteriology Virology Service, Medical Biology Laboratory. Moulay Ismail Military Hospital., Bacteriology Virology Service. Meknès, MAR
Abstract
Background
Tuberculosis is a ubiquitous, contagious infectious disease caused by the Mycobacterium tuberculosis complex (MTC), it constitutes a major public health problem both nationally and internationally. Unfortunately, what has made the disease even more challenging to manage is the development of resistance to various first-line antitubercular drugs, The main objective of this study is to describe the epidemiological profile of (MDR-TB) in the Meknes prefecture, Fes-Meknes region.
Methods
This is a cross-sectional study of MDR-TB cases monitored at the Tuberculosis and Respiratory Disease Diagnostic Center (CDTMR) in the city of Meknes, Fez-Meknes region. Data collection was conducted over a period spanning from January 2017 to December 2022 (6 years).
Results
The study analyzed 28 cases of MDR-TB in Meknes Prefecture, revealing a predominantly young (mean age: 17.32 years) and male population (85.7%), with most patients residing in urban areas (85.7%). Nearly all cases (99%) were smear-positive. Treatment durations varied: 50% underwent 24 months, 46.4% completed 11 months, and 3.6% received six months. The mortality rate was 10.7%, with three deaths, while 89.3% of patients survived. Relapse occurred in 32.1% of cases. Risk factors were prevalent, with 75% of patients having at least one; smoking was reported in 53.6% of cases, suggesting its role in disease progression. The bivariate analysis explored factors associated with mortality in individuals with MDR-TB. The overall mortality rate was 10.7%. Gender, residence, relapse history, diabetes, and HIV were not associated with mortality (all p > 0.05). Notably, sensory side effects showed a significant association with mortality (p = 0.008).
Conclusions
Managing MDR-TB requires addressing comorbidities, mitigating side effects, and improving adherence through equitable healthcare interventions. Future efforts should focus on bridging rural access gaps and targeting behavioral health determinants.

Leave A Comment