Conference 2021 Poster Presentation
Project title
Moroccan Scleroderma patients with Anti-mitochondrial antibodies
Authors and Affiliations
Zeineb Zian1, Khaoula Hamdouch1,2, Mouna Maamer3, Amina Barakat1, Naima Ghailini Nourouti1, Manuel Valdivia2, Mohcine Bennani Mechita1, Naima Arji4
1. Biomedical Genomics and Oncogenetics Research Laboratory, Department of Biology, Faculty of Sciences and Techniques of Tangier, Abdelmalek Essaadi University, Morocco.
2. Department of Biomedicine, Biotechnology and Public Health, Faculty of Sciences, University of Cadiz, Cadiz, Spain.
3. Internal Medicine Department, Hospital Ibn Sina, Rabat, Morocco.
4. Autoimmunity Laboratory, National Institute of Hygiene, Rabat, Morocco.
Abstract
Background
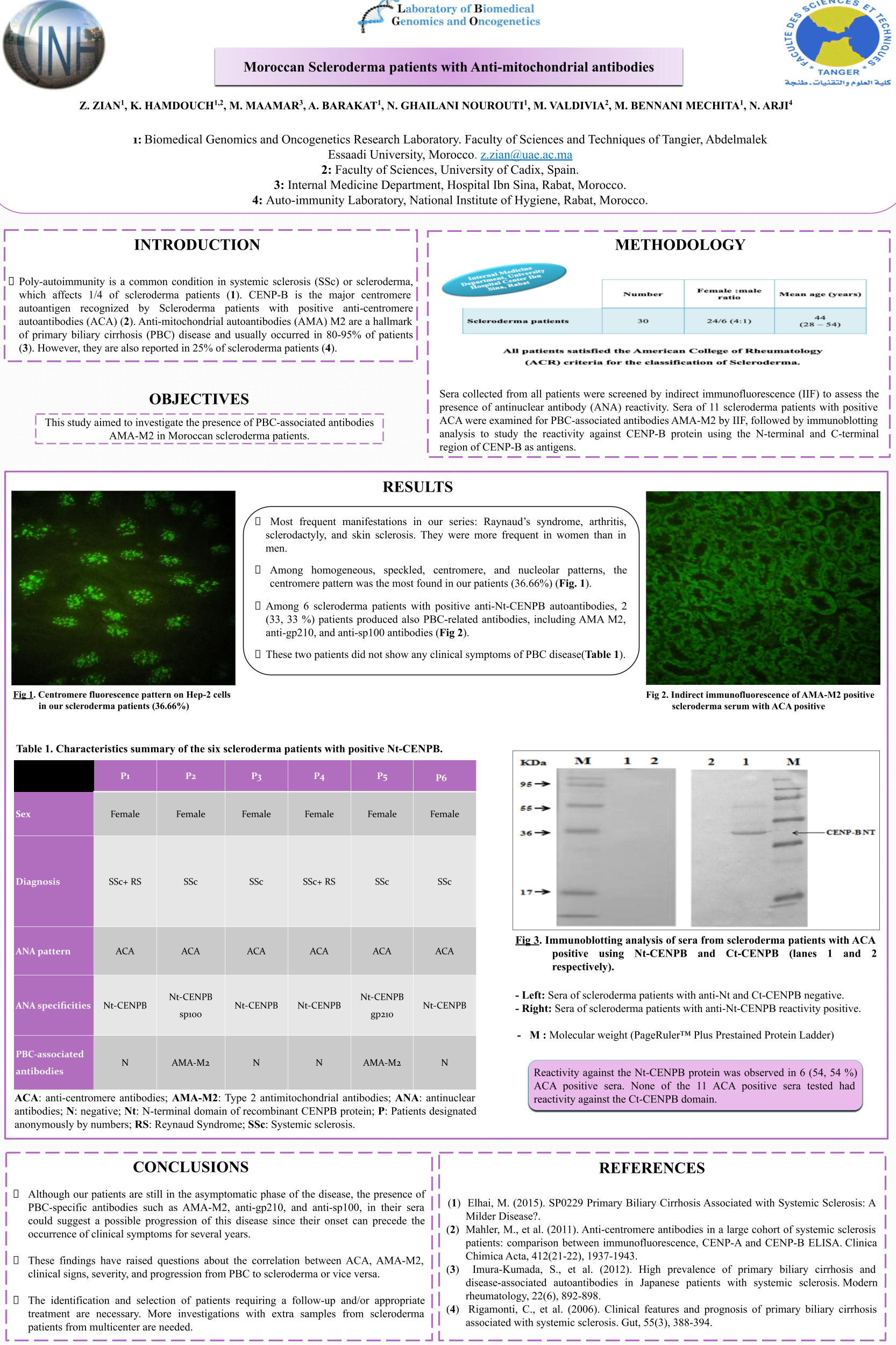
Anti-mitochondrial auto-antibodies (AMA) are considered as a hallmark of Primary Biliary Cirrhosis (PBC) disease and usually occurred in 80-95% of patients. Although the prevalence of PBC among scleroderma patients has been estimated to 3%, AMA have been also reported in 25% of scleroderma patients. Our objective was to investigate the presence of PBC-associated antibodies AMA-M2 in sera from 30 Moroccan scleroderma patients recruited between December 2011 and December 2013 from the University Hospital Center of Rabat-Morocco.
Methods
Sera collected from all patients were screened by indirect immunofluorescence (IIF) to assess the presence of antinuclear antibodies (ANA) reactivity. Sera of 11 scleroderma patients with positive ACA were examined for PBC-associated antibodies AMA-M2 by IIF, followed by immunoblotting analysis to study the reactivity against CENP-B protein using the N-terminal and C-terminal region of CENP-B as antigens.
Results
The female to male ratio was 4:1, and the mean age was 44 years. Of 30 scleroderma patients, 11 (36.67%) patients were positive for ACA, and 6 of them (54.54%) produced auto-antibodies against Nt-CENPB antigen. Among these six patients with anti-Nt-CENPB antibodies, two (33. 33 %) patients produced also other PBC-related antibodies, such as AMA M2, anti-gp210, and anti-sp100 antibodies. These two patients neither diagnosed with PBC nor showed any clinical symptoms for this disease.
Conclusions
Our results may be of great value suggesting an increased risk of scleroderma patients developing PBC disease. These preliminary findings have raised questions about the correlation between ACA, AMA-M2, clinical signs, severity, and progression from PBC to scleroderma or vice versa. Further studies from multicenter are warranted to confirm and validate these results.